Anatomy
Common Conditions
The cornea is the front window of the eye. It is a transparent tissue that covers the iris, pupil, and anterior chamber. Since transparency of the cornea is so important to vision, it has no blood vessels and no blood supply. Oxygen is directly absorbed through the air. We make sure the cornea remains transparent, avascular, and protected from infection so the window remains healthy and clear.
The lens is a biconvex structure within the eye that helps the cornea focus light. Similar to a lens of a camera, it changes the way light bends as it enters the eye. The lens is also transparent, but does tend to become less transparent over time due to aging and sun exposure. We check the lens regularly to make sure the lens does not develop opacities that can hinder vision.
The retina is a thin tissue lining the back surface of the eye like wallpaper. It can be analogous to the film in a camera. The retinal tissue absorbs all the light entering the eye and transmits all that information to the brain via an electrical cable known as the optic nerve. Since the retina has no pain receptors, there are no symptoms associated with retinal diseases until vision loss is perceived. We check to make sure the retinal tissue is stable and healthy at every check up.
What is glaucoma?
Glaucoma is a disease of the optic nerve – the electrical cable that connects the eye to the brain. Within this electrical cable there are numerous electrical wires, carrying light information to our brain. When damage to the electrical wires (optic nerve fibers) occurs, blind spots develop. These blind spots usually go undetected until the optic nerve is significantly damaged. If the entire nerve is destroyed, blindness results.
Early detection and treatment are the keys to preventing optic nerve damage and blindness from glaucoma. Glaucoma is a leading cause of blindness in the United States, especially for older people. But loss of sight from glaucoma can often be prevented with early treatment.
What causes glaucoma?
Clear liquid called aqueous humor is constantly being produced inside the eye. In order to maintain a healthy level of pressure within the eye, the fluid being produced has to also be able to flow out of the eye through a microscopic drainage system. Since the eye is a closed structure, if the fluid is produced faster than it is drained, the pressure inside the eye can increase rapidly. Similarly if the drain is ‘clogged’, the pressure can also build up inside the eye. The pressure could increase to a point where it starts damaging the optic nerve, leading to blindness if undetected.
How is glaucoma detected?
Regular eye examinations are critical to detecting glaucoma. Since there are no pain receptors at the optic nerve, it is rare to feel or see any changes in your vision until the optic nerve is severely damaged. During a typical glaucoma evaluation, we will:
Photography of the optic nerve or other computerized imaging may be recommended.
How is glaucoma treated?
Damage to the optic nerve from glaucoma cannot be reversed. Eyedrops, laser surgery, and surgery in the operating room are methods used to lower eye pressure and help prevent further damage. In some cases, oral medications may also be prescribed.
With any type of glaucoma, periodic examinations are very important to prevent vision loss. Because glaucoma can progress without your knowledge, adjustments to your treatment may be necessary from time to time.
What is a cataract?
A cataract is typically a natural clouding and yellowing of the clear lens inside the eye. It can be compared to a window that is frosted or yellowed. The amount and pattern of cloudiness within the lens can vary. One’s vision will also vary, depending on the location and the extent of the opacification. Common symptoms of cataract include: a painless, gradual blurring of vision, glare, light sensitivity, poor night vision, double vision in one eye, needing brighter light to read, fading or yellowing of colors.
What causes cataract?
The most common type of cataract is related to aging of the eye. Other causes of cataract include: family history, medical problems (such as diabetes), injury to the eye, medications (especially steroids), radiation, long-term unprotected exposure to sunlight, previous eye surgery, or unknown factors.
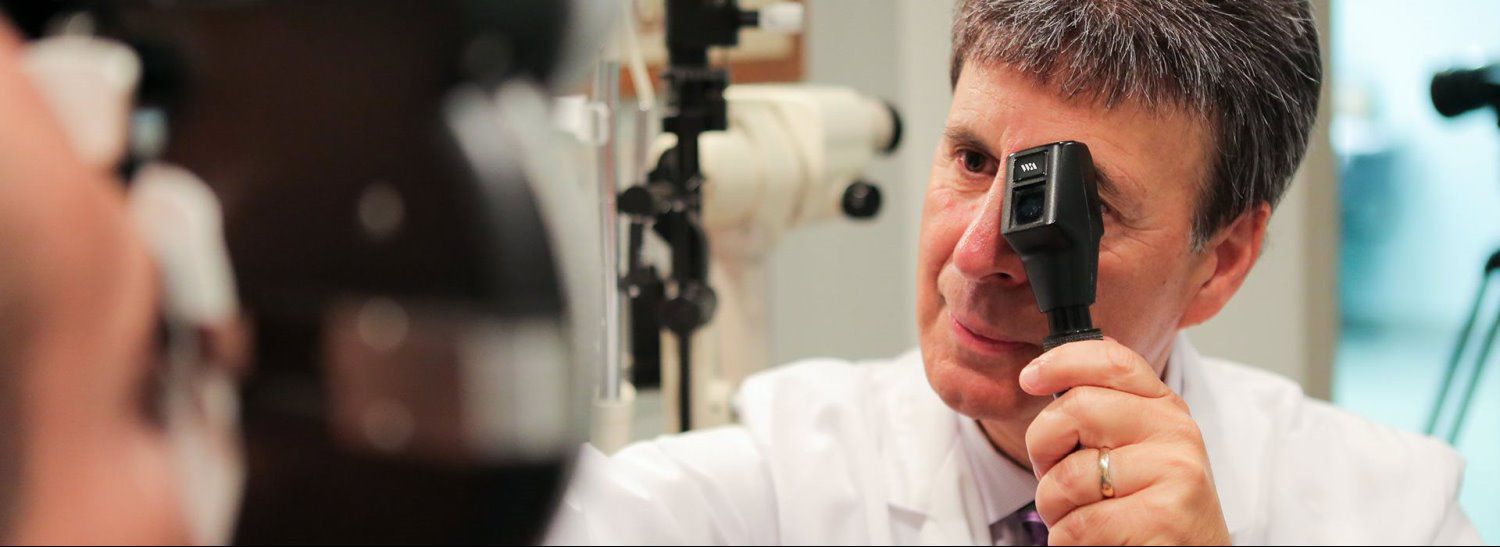
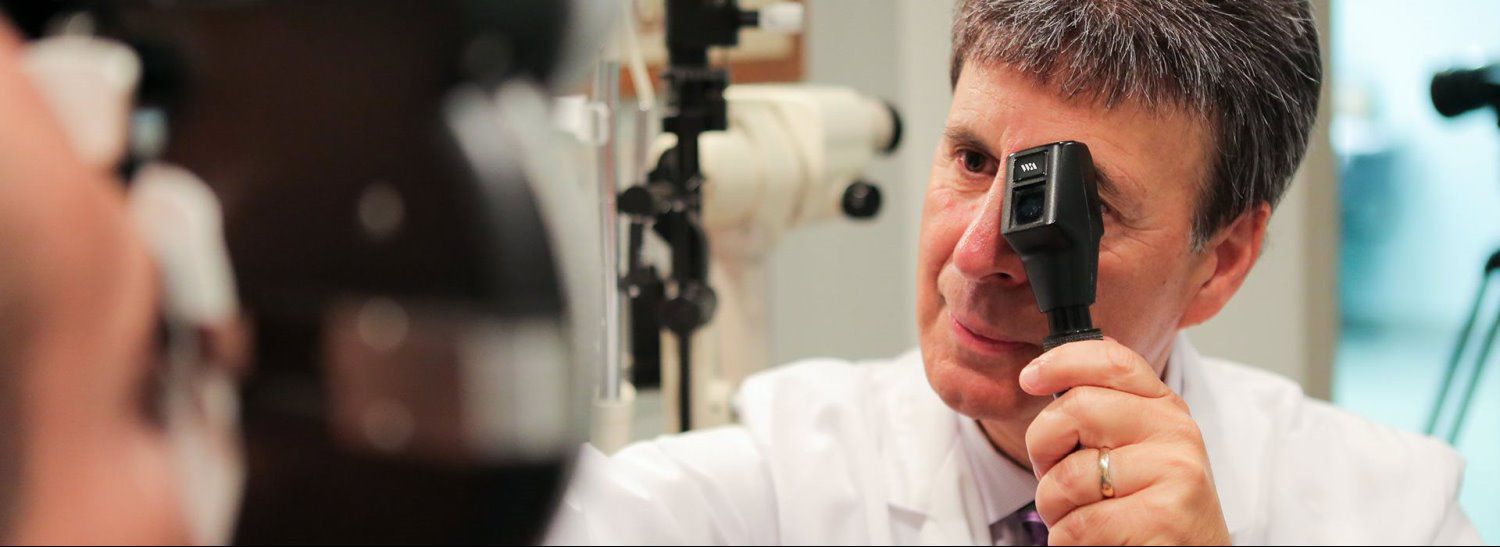
How is a cataract detected?
Presence of a cataract is detected by performing a thorough eye examination. A careful evaluation using a high-powered microscope will allow us to see any clouding or opacifications in the lens. When the development of the cataract begins to hinder functional vision, cataract removal may be recommended.
How is a cataract treated?
Surgery is the only way a cataract can be removed. However, if the symptoms of cataract are not bothering you very much, surgery may not be needed. Sometimes a simple change in your eyeglass prescription may be helpful. No medications, dietary supplements or exercises have been shown to prevent or cure cataracts. Protection from excessive sunlight may help slow the progression of cataracts. Sunglasses that screen out ultraviolet (UV) light rays or regular eyeglasses with a clear anti-UV coating offer this protection.
Diabetic retinopathy is a condition in which diabetes begins to affect the blood vessels inside the eye. There are two types of diabetic retinopathy: non-proliferative (NPDR) and proliferative (PDR) diabetic retinopathy. NPDR involves leaking of blood or fluid from tiny blood vessels within the retina. This usually causes swelling in the retinal tissue (edema) or deposits to form (exudates). This can lead to changes, or even loss of vision due to retinal edema or ischemia (loss of blood supply). PDR involves the body’s own natural attempt to bring nutrients to ischemic tissue by creating new blood vessels, also known as neovascularization. The problem with these new blood vessels is that they leak very easily, and cause even more damage to the retinal tissue, such as retinal detachments, neovascular glaucoma, and vitreous hemorrhaging.
What causes diabetic retinopathy?
Diabetic retinopathy is caused by systemic diabetes. A large majority of people with diabetes will have some form of mild NPDR, even though it has not affected vision yet. The longer a person is diagnosed with diabetes, the more likely they will develop diabetic retinopathy.
How is diabetic retinopathy detected?
It is crucial for all diabetics to have a comprehensive retinal evaluation at least once every year. Retinal photographs or dilated retinal exams are recommended for all diabetics. Flourescein angiography may also be indicated to evaluate abnormal blood vessel growth and retinal edema.
How is diabetic retinopathy treated?
Treatment of diabetic retinopathy varies depending on the severity of the retinopathy. Blood sugar control is critical in preventing or slowing the progression of retinopathy. Mild NPDR usually only involves close monitoring of the retinal tissue, as well as diet and exercise to control blood sugar levels. Laser treatment may be used to treat any leakage of blood or fluid from weak blood vessels in more advanced stages of diabetic retinopathy. Sometimes, surgical procedures such as vitrectomies may be needed.
What is dry eye syndrome?
One of the most common conditions that we see in this day and age is dry eye. Dry eyes are caused by a wide array of reasons, and also have a varying degree of symptoms. It is generally characterized by burning, itching, red eyes. This occurs when the eyes are either not producing enough tears to moisturize the eye, or when the tears themselves evaporate faster than it is being replaced. Dry eye not only can cause the eyes to look red and irritated, but it can also make the eyes feel sandy and gritty, and cause them to constantly water and tear.
What causes dry eye syndrome?
Environmental factors such as allergens, smoke, pollutants, air conditioning, heat, or even living in a dry area can cause dry eye syndrome. Being on the computer, normal aging, and not staying hydrated enough are also very common causes of dry eye, along with contact lens wear, systemic medications, conditions or injuries.
How is dry eye detected?
Try answering our dry eye questionnaire found on our FORMS page. During our comprehensive eye exam, we make sure the tears are producing normally, and staying on the surface of the eye for an adequate amount of time. We also check to make sure the eyelids are functioning properly and for any other conditions that could cause dry eye.
How is dry eye treated?
Dry eyes are usually treated homeopathically first, from drinking more water, resting the eyes while on the computer, to using humidifiers and/or artificial tears at home or at work. If the dryness does not improve using these methods, medications may be used, or plugs could be inserted into the tear ducts to slow the drainage of tears from the eyes. Treatment of the eyelid could also be included in treating dry eye since eyelids play such a big role in maintaining tear function.
What is age-related macular degeneration?
Age-related macular degeneration (AMD) is the leading cause of vision loss in people 50 years or older in the United States. It involves damage to the part of the eye called the macula: a small but extremely important area of the retina. The macula is responsible for all of the eye’s central and detailed vision. The majority of AMD cases involve the ‘dry’ form, a slow progressing change in the macular tissue. If left unmonitored, the dry form can progress to the more severe ‘wet’ form.
What causes age-related macular degeneration?
Besides normal age-related changes, ultraviolet light exposure is also known to accelerate damage to the macular tissue. Just like sunbathing without sunscreen, the more UV exposure the skin gets, the more damaged it gets. Similarly, without the protection of sunglasses, especially around water and snow, the macula also gets damaged from too much UV exposure. Heredity, high blood pressure, cardiovascular disease, and smoking are also risk factors.
How is age-related macular degeneration detected?
Utilizing modern technological advances such as the Optomap® panoramic retinal camera allows us to monitor any subtle changes in the retinal tissue, including early signs of macular degeneration. A thorough evaluation of the macula, either with the Optomap® retinal camera, or by dilation, is included in every comprehensive eye examination.
How is age-related macular degeneration treated?
There are currently no forms of treatment for ‘dry’ AMD. However, it is important to monitor changes regularly and slow or stop progression towards ‘wet’ AMD. Anti-oxidants such as vitamins A, C, and E, along with zinc, zeaxanthin, and lutein have been shown to slow the progression of dry AMD. As for wet AMD, there are advanced diagnostic techniques and drug therapies currently used for treatment, and much more to come.
What is blepharitis?
Blepharitis is a chronic inflammatory eyelid condition, characterized by crusting, flaking, swollen and red eyelid margins. Vision may also be intermittently blurry, and tear frequently, due to secondary dry eyes.
What causes blepharitis?
Blepharitis is caused by a variety of triggers. The most common are hereditary conditions such as rosacea, inflammatory conditions such as allergy, contact lens wear, and poor lid hygiene.
How is blepharitis detected?
Using a high-powered microscope, we are able to assess the delicate structure of the lid margins for any abnormalities, such as swelling, inflammatory reactions, or clogged oil glands that can ultimately lead to chronic blepharitis.
How is blepharitis treated?
Depending on the severity of the condition, typically a combination of warm compresses, eyelid scrubs, dry eye therapies, and/or antibiotics are used to treat blepharitis.
What is conjunctivitis?
Conjunctivitis is a fairly common condition in which the outermost layer of the eye and inner surface of the lids (conjunctiva) gets irritated and inflamed.
What causes conjunctivitis?
The most common causes of conjunctivitis are allergies, or infections (either viral or bacterial). Both bacterial and viral infections are contagious, usually transmitted person-to-person, or through contaminated objects.
How is conjunctivitis detected?
Conjunctivitis symptoms range from mild to severe, depending on the cause. These symptoms can involve itching, light sensitivity, discharge, redness, tearing, and sometimes pain and blurring of vision. A high-powered microscope is used to determine the cause of the conjunctivitis, as well as to rule out any other possible causes such as glaucoma, uveitis or keratitis.
How is conjunctivitis treated?
Allergic conjunctivitis is typically treated with cold compresses, and/or allergy medication, and ultimately removal of the allergen source (if possible). Viral and bacterial conjunctivitis are usually treated with cold compresses, and/or prophylactic antibiotics to limit the extent of infection.
What is astigmatism?
Astigmatism is a common optical condition in which the front surface of the eye is not spherical, like a baseball, but more oval, like an egg or a football. This in turn causes the light coming into the eye to focus at two different distances. So instead of seeing one image, there are two images overlapped next to each other. This creates blur, especially at nighttime or in dim lighting conditions.
What causes astigmatism?
Astigmatism is due to the natural development of the eye, similar to myopia (near-sightedness) and hyperopia (far-sightedness). Hereditary factors have been shown to play roles in the development of astigmatism.
How is astigmatism detected?
Using different techniques, we are able to detect the presence, location, and amount of astigmatism in the eye. These techniques include retinoscopy, keratometry and refraction. A corneal topographer may also be used to create a topographical map of the front surface of the eye.
How is astigmatism treated?
Astigmatism is corrected with eyeglasses and/or contact lenses. Specialty contact lenses, both soft and hard, are available to correct different degrees of astigmatism. In some cases, specific specialty lenses are needed to correct certain types of astigmatism. Refractive surgery is also another alternative, depending on the location and amount of astigmatism present.